What Will Cause Feet To Over Pronate
Over-pronation occurs when the foot collapses too far inward stressing the plantar fascia (the area underneath the arch of the foot.) Normally, one pronates every time he/she walks, but excessive pronation is called over-pronation. When this occurs it can cause pain in the feet, knees, hips, low back and even the shoulder.
Causes
Over-pronation is very prominent in people who have flexible, flat feet. The framework of the foot begins to collapse, causing the foot to flatten and adding additional stress to other parts of the foot. Therefore over-pronation can often lead to a case of Plantar Fasciitis, Heel Spurs, Metatarsalgia, Post-tib Tendonitis and/or Bunions. There are many causes of flat feet. Obesity, pregnancy or repetitive pounding on a hard surface can weaken the arch leading to over-pronation. People with flat feet often do not experience discomfort immediately, and some never suffer from any discomfort at all. However, when symptoms develop and become painful, walking becomes awkward and causes increased strain on the feet and calves.
Symptoms
Over-pronation is a condition where the arch flattens out which makes the feet roll inward while walking. This condition is also known as flat feet. It imposes extreme additional stresses on the plantar fascia, a fibrous band of tissue which connects the heel to the forefoot. Over-pronation makes walking a painful experience because of the additional strain on the calves, heel and/or back. Treatment for over-pronation involves the use of specially-made orthotics which offers arch support and medial rear foot posting as corrective measures.
Diagnosis
People who overpronate have flat feet or collapsed arches. You can tell whether you overpronate by wetting your feet and standing on a dry, flat surface. If your footprint looks complete, you probably overpronate. Another way to determine whether you have this condition is to simply look at your feet when you stand. If there is no arch on the innermost part of your sole, and it touches the floor, you likely overpronate. The only way to truly know for sure, however, is to be properly diagnosed by a foot and ankle specialist.

Non Surgical Treatment
Overpronation is a condition in which the foot rolls excessively down and inward. The arch may elongate and collapse (or ?fall?) and the heel will lean inward. Overpronation should not be confused with pronation. Pronation is a normal motion of the foot during weight bearing and allows the foot to absorb shock as it contacts the ground.
Surgical Treatment
Hyperpronation can only be properly corrected by internally stabilizing the ankle bone on the hindfoot bones. Several options are available. Extra-Osseous TaloTarsal Stabilization (EOTTS) There are two types of EOTTS procedures. Both are minimally invasive with no cutting or screwing into bone, and therefore have relatively short recovery times. Both are fully reversible should complications arise, such as intolerance to the correction or prolonged pain. However, the risks/benefits and potential candidates vary. Subtalar Arthroereisis. An implant is pushed into the foot to block the excessive motion of the ankle bone. Generally only used in pediatric patients and in combination with other procedures, such as tendon lengthening. Reported removal rates vary from 38% - 100%, depending on manufacturer. HyProCure Implant. A stent is placed into a naturally occurring space between the ankle bone and the heel bone/midfoot bone. The stent realigns the surfaces of the bones, allowing normal joint function. Generally tolerated in both pediatric and adult patients, with or without adjunct soft tissue procedures. Reported removal rates, published in scientific journals vary from 1%-6%.
Does Severs Disease Call For Surgical Treatment?
Sever?s disease is a condition occurring in pre-adolescents that causes pain, swelling and soreness in the heel bone, also known as the calcaneus. Sever?s disease causes pain on either side of and/or on the bottom of the heel. During a period of pre-adolescent development, the growing heel bone can be overused when the child is involved in a lot of running and jumping activities. Impact on the heel bone and repeated traction on the growing bone from the Achilles tendon can lead to swelling in the area.
Causes
During the growth spurt of early puberty, the bones often grow faster than the leg muscles and tendons. This can cause the muscles to become very tight and overstretched, the heel becomes less flexible and this build-up of pressure can result in redness, swelling, tenderness and pain at the heel.
Symptoms
The symptoms of Sever?s disease occur in the heel and the foot, and may worsen with activity. Pain and stiffness can occur in one or both heels. Symptoms can include. Swelling in the heel. Redness in the heel. Antalgic gait (such as limping). Foot pain or stiffness first thing in the morning or while walking. Pain that is worsened by squeezing the heel.
Diagnosis
Your Podiatrist or Physiotherapist will assist in diagnosing the injury and the extent of the damage. From this, they will develop a management plan which may include rest or activity modification, soft tissue treatment such as massage and stretching, correction of biomechanics through heel raises or orthoses and the progression through a series of specific strengthening exercises.
Non Surgical Treatment
Depending on the Podiatrist's diagnosis and the severity of the pain, there are several treatment options available. Rest/ reduced activity: your child should reduce or stop any activity that causes pain, such as sports and running. This can be a difficult option, as children are normally quite willful in pursuit of their favorite pastimes! Over the counter anti-inflammatory drugs, such as ibuprofen (found in Nurofen), to help reduce pain and inflammation. Try to make sure your child does the recommended stretching exercises before sport/play. This will should help reduce the stress on the fascia tendon and relieve heel pain. The use of Orthotic insoles. Footactive Kids orthotics are made for children. They will help properly support the foot, help prevent over-pronation or improper gait restoring your child's foot the the correct biomechanical position. If you are in any doubt or your child's foot pain persists then please arrange an appointment with a Podiatrist or Physiotherapist. Please click here for more information on the use of orthotics for children.
What Can Cause Posterior Tibial Tendon Dysfunction ?
Overview
Posterior tibial tendon insufficiency (also called posterior tibial tendon dysfunction or adult acquired flatfoot) has been named literally after failure of the posterior tibial tendon. However, the condition is caused not only by the progressive failure of the posterior tibial tendon; it is also failure of associated ligaments and joints on the inner side of the ankle and foot. This results in collapse of the arch of the foot, along with the deformity which most often becomes the debilitating problem in its later stages. While at the beginning the common symptom is pain over the tendon in the inner part of the hindfoot and midfoot, later on it is the deformity that can threaten a person?s ability to walk. Just as the tendon degenerates and loses its function, other soft tissue on the same inner side of the foot - namely the ligaments - degenerate and fail. Ligaments are responsible for holding bones in place, and when they fail, bones shift to places where they shouldn?t; deformity is the result. The deformity causes malalignment, leading to more stress and failure of the ligaments. 
Causes
Flat footedness, most people who develop the condition already have flat feet. With overuse or continuous loading, a change occurs where the arch begins to flatten more than before, with pain and swelling developing on the inside of the ankle. Inadequate support from footwear may occasionally be a contributing factor. Trauma or injury, occasionally this condition may be due to fracture, sprain or direct blow to the tendon. Age, the risk of developing Posterior Tibial Tendon Dysfunction increases with age and research has suggested that middle aged women are more commonly affected. Other possible contributing factors - being overweight and inflammatory arthritis.
Symptoms
Many patients with this condition have no pain or symptoms. When problems do arise, the good news is that acquired flatfoot treatment is often very effective. Initially, it will be important to rest and avoid activities that worsen the pain.
Diagnosis
It is of great importance to have a full evaluation, by a foot and ankle specialist with expertise in addressing complex flatfoot deformities. No two flat feet are alike; therefore, "Universal" treatment plans do not exist for the Adult Flatfoot. It is important to have a custom treatment plan that is tailored to your specific foot. That starts by first understanding all the intricacies of your foot, through an extensive evaluation. X-rays of the foot and ankle are standard, and MRI may be used to better assess the quality of the PT Tendon.
Non surgical Treatment
Get treated early. There is no recommended home treatment. While in stage one of the deformity, rest, a cast, and anti-inflammatory therapy can help you find relief. This treatment is followed by creating custom-molded foot orthoses and orthopedic footwear. These customized items are critical in maintaining the stability of the foot and ankle. Once the tendon has stretched and deformity is visible, the chances of success for non-surgical treatment are significantly lower. In a small percentage of patients, total immobilization may arrest the progression of the deformity. A long-term brace known as an ankle foot orthosis is required to keep the deformity from progressing. The Richie Brace, a type of ankle foot orthosis, shows significant success as a treatment for stage two posterior tibial dysfunction. It is a sport-style brace connected to a custom corrected foot orthodic that fits into most lace-up footwear (including athletic shoes). It is also light weight and more cosmetically appealing than traditionally prescribed ankle foot orthosis. The Arizona Brace, California Brace or Gauntlet Brace may also be recommended depending on your needs. 
Surgical Treatment
If cast immobilization fails, surgery is the next alternative. Treatment goals include eliminating pain, halting deformity progression and improving mobility. Subtalar Arthroereisis, 15 minute outpatient procedure, may correct flexible flatfoot deformity (hyperpronation). The procedure involves placing an implant under the ankle joint (sinus tarsi) to prevent abnormal motion. Very little recovery time is required and it is completely reversible if necessary. Ask your Dallas foot doctor for more information about this exciting treatment possibility.
Arch Pain
Arch pain (medically known as plantar pain) is a broad term many people use to describe pain in their muscles, tendons, ligaments, bones, or nerves. All these components are connected to the bottom of the foot; therefore, damage to any one of these can cause pain on the bottom of the foot. This pain may only last for short time, but can progressively worsen if untreated. Most people who suffer from this pain are between the ages of 30 and 80, but many younger athletes are also susceptible, particularly those who participate in high-impact sports.

Causes
The normal arch is made up of bones and joints, which are held tightly together, in a precise relationship. When this relationship is subjected to repeated abnormal weight, or the normal weight of a lifetime, the force breaks up this normal relationship, causing bones to shift and joints to buckle. This allows the arch to collapse, and produces pain. The ability of the arch to absorb the shock of each step is reduced, so that continued walking will eventually produce pain in the knee, hip, and lower back. All four of the above categories will eventually cause this to happen. Arch pain can also be a manifestation of heel spur or nerve injury in the heel area. There are also certain types of benign growths that can cause arch pain i.e. Plantar fibromatosis.
Symptoms
The foot of a newborn with congenital vertical talus typically has a convex rocker-bottom shape. This is sometimes combined with an actual fold in the middle of the foot. The rare person who is diagnosed at an older age often has a "peg-leg" gait, poor balance and heavy calluses on the soles where the arch would normally be. If a child with congenital vertical talus has a genetic disorder, additional symptoms often are seen in other parts of the body.
Diagnosis
In more difficult cases of plantar fasciitis you should see your foot health professional for a thorough examination. They will find out why your arch or heel pain occurred in the first place and devise a treatment plan to relieve your pain and prevent it from reoccurring. They will evaluate your feet, walking pattern (gait), shoes, activities, exercise methods, and other relevant information and then devise your treatment plan.
Non Surgical Treatment
For mild pain or aching, acetaminophen (Tylenol) or a nonsteroidal anti-inflammatory drug (NSAID), such as aspirin or ibuprofen (Advil, Motrin and others) may be effective. When there are no symptoms, treatment is not needed. If a child older than age 3 develops symptoms, the doctor may prescribe a therapeutic shoe insert made from a mold of the child's foot or a corrective shoe. As an alternative, some doctors recommend store-bought arch supports. These appear to work as well as more expensive treatments in many children. With any conservative, nonsurgical treatment, the goal is to relieve pain by supporting the arch and correcting any imbalance in the mechanics of the foot. Surgery is typically offered as a last resort in people with significant pain that is resistant to other therapies.

Surgical Treatment
Surgical advances have dramatically improved the ability to alleviate the pain and decreased function that millions of Americans experience due to flat feet. Nevertheless, many patients and even some physicians remain unaware of the new procedures, which are best performed by a foot and ankle specialist who has the applicable training and experience.
Prevention
There are several things that you can do to prevent and treat arch pain. This includes Avoiding high heeled shoes, Stretching the calf muscles regularly, Wearing well fitted, comfortable shoes, Using customisedorthotic devices or shoe inserts, Elevating the feet and applying ice and taking over-the-counter anti-inflammatory medications. You can also care for your feet by paying attention to any changes in your feet as you get older. It is normal for feet to lose some of their fat pads as a person ages. Your feet may get bigger, both wider and longer as well. Make sure that you wear shoes that are sturdy, but comfortable, and have your feet measured before you buy shoes to make sure that you are still wearing the right size. Shoe sizes vary from one brand to the next, so it is a good idea to have your feet measured every time you purchase shoes. When choosing shoes, match the shoe to the activity for which it will be worn. Within the broader grouping of athletic shoes, there are different categories with different features. For example, a running shoe has different features than a walking shoe. You may develop some arthritic changes in your feet over time, too. If you notice that you are experiencing more pain in your feet, see your doctor for an evaluation. If the pain is arthritis-related, your doctor may recommend medication or other treatment to slow the progression of the arthritis.
Stretching Exercises
Flexibility is important in preventing injuries. With a simple stretching exercise, you can rehabilitate the muscles of your foot to relieve arch pain and prevent future injuries. This simple exercise by Tammy White and Phyllis Clapis for Relay Health is a good way to strengthen your foot muscles and stretch your plantar fascia. Sit in a chair and cross one foot over your other knee. Grab the base of your toes and pull them back toward your leg until you feel a comfortable stretch. Hold 15 seconds and repeat three times. When you can stand comfortably on your injured foot, you can begin standing to stretch the plantar fascia at the bottom of your foot.
■
Overview
PTTD is most commonly seen in adults and referred to as "adult acquired flatfoot". Symptoms include pain and swelling along the inside arch and ankle, loss of the arch height and an outward sway of the foot. If not treated early, the condition progresses to increased flattening of the arch, increased inward roll of the ankle and deterioration of the posterior tibial tendon. Often, with end stage complications, severe arthritis may develop. How does all this happen? In the majority of cases, it is overuse of the posterior tibial tendon that causes PTTD. And it is your inherited foot type that may cause a higher possibility that you will develop this condition. 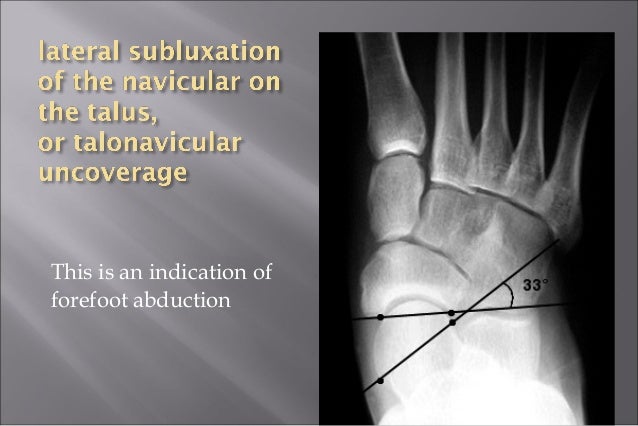
Causes
A person with flat feet has greater load placed on the posterior tibial tendon which is the main tendon unit supporting up the arch of the foot. Throughout life, aging leads to decreased strength of muscles, tendons and ligaments. The blood supply diminishes to tendons with aging as arteries narrow. Heavier, obese patients have more weight on the arch and have greater narrowing of arteries due to atherosclerosis. In some people, the posterior tibial tendon finally gives out or tears. This is not a sudden event in most cases. Rather, it is a slow, gradual stretching followed by inflammation and degeneration of the tendon. Once the posterior tibial tendon stretches, the ligaments of the arch stretch and tear. The bones of the arch then move out of position with body weight pressing down from above. The foot rotates inward at the ankle in a movement called pronation. The arch appears collapsed, and the heel bone is tilted to the inside. The deformity can progress until the foot literally dislocates outward from under the ankle joint.
Symptoms
Patients often experience pain and/or deformity at the ankle or hindfoot. When the posterior tibial tendon does not work properly, a number of changes can occur to the foot and ankle. In the earlier stages, symptoms often include pain and tenderness along the posterior tibial tendon behind the inside of the ankle. As the tendon progressively fails, deformity of the foot and ankle may occur. This deformity can include progressive flattening of the arch, shifting of the heel so that it no longer is aligned underneath the rest of the leg, rotation and deformity of the forefoot, tightening of the heel cord, development of arthritis, and deformity of the ankle joint. At certain stages of this disorder, pain may shift from the inside to the outside aspect of the ankle as the heel shifts outward and structures are pinched laterally.
Diagnosis
Although you can do the "wet test" at home, a thorough examination by a doctor will be needed to identify why the flatfoot developed. Possible causes include a congenital abnormality, a bone fracture or dislocation, a torn or stretched tendon, arthritis or neurologic weakness. For example, an inability to rise up on your toes while standing on the affected foot may indicate damage to the posterior tibial tendon (PTT), which supports the heel and forms the arch. If "too many toes" show on the outside of your foot when the doctor views you from the rear, your shinbone (tibia) may be sliding off the anklebone (talus), another indicator of damage to the PTT. Be sure to wear your regular shoes to the examination. An irregular wear pattern on the bottom of the shoe is another indicator of acquired adult flatfoot. Your physician may request X-rays to see how the bones of your feet are aligned. Muscle and tendon strength are tested by asking you to move the foot while the doctor holds it.
Non surgical Treatment
Because of the progressive nature of PTTD, early treatment is advised. If treated early enough, your symptoms may resolve without the need for surgery and progression of your condition can be arrested. In contrast, untreated PTTD could leave you with an extremely flat foot, painful arthritis in the foot and ankle, and increasing limitations on walking, running, or other activities. In many cases of PTTD, treatment can begin with non-surgical approaches that may include. Orthotic devices or bracing. To give your arch the support it needs, your foot and ankle surgeon may provide you with an ankle brace or a custom orthotic device that fits into the shoe. Immobilization. Sometimes a short-leg cast or boot is worn to immobilize the foot and allow the tendon to heal, or you may need to completely avoid all weight-bearing for a while. Physical therapy. Ultrasound therapy and exercises may help rehabilitate the tendon and muscle following immobilization. Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation. Shoe modifications. Your foot and ankle surgeon may advise changes to make with your shoes and may provide special inserts designed to improve arch support. 
Surgical Treatment
In cases of PTTD that have progressed substantially or have failed to improve with non-surgical treatment, surgery may be required. For some advanced cases, surgery may be the only option. Surgical treatment may include repairing the tendon, tendon transfers, realigning the bones of the foot, joint fusions, or both. Dr. Piccarelli will determine the best approach for your specific case. A variety of surgical techniques is available to correct flexible flatfoot. Your case may require one procedure or a combination of procedures. All of these surgical techniques are aimed at relieving the symptoms and improving foot function. Among these procedures are tendon transfers or tendon lengthening procedures, realignment of one or more bones, or insertion of implant devices. Whether you have flexible flatfoot or PTTD, to select the procedure or combination of procedures for your particular case, Dr. Piccarelli will take into consideration the extent of your deformity based on the x-ray findings, your age, your activity level, and other factors. The length of the recovery period will vary, depending on the procedure or procedures performed.
The Causes And Treatments
Overview
The posterior tibialis muscle originates on the bones of the leg (tibia and fibula). This muscle then passes behind the medial (inside) aspect of the ankle and attaches to the medial midfoot as the posterior tibial tendon. The posterior tibial tendon serves to invert (roll inward) the foot and maintain the arch of the foot. This tendon plays a central role in maintaining the normal alignment of the foot and also in enabling normal gait (walking). In addition to tendons running across the ankle and foot joints, a number of ligaments span and stabilize these joints. The ligaments at the medial ankle can become stretched and contribute to the progressive flattening of the arch. Several muscles and tendons around the ankle and foot act to counter-balance the action of the posterior tibial tendon. Under normal circumstances, the result is a balanced ankle and foot with normal motion. When the posterior tibial tendon fails, the other muscles and tendons become relatively over-powering. These muscles then contribute to the progressive deformity seen with this disorder. 
Causes
Several risk factors are associated with PTT dysfunction, including high blood pressure, obesity, diabetes, previous ankle surgery or trauma and exposure to steroids. A person who suspects that they are suffering from PTT dysfunction should seek medical attention earlier rather than later. It is much easier to treat early and avoid a collapsed arch than it is to repair one. When the pain first happens and there is no significant flatfoot deformity, initial treatments include rest, oral anti-inflammatory medications and, depending on the severity, a special boot or brace.
Symptoms
Some symptoms of adult acquired flat foot are pain along the inside of the foot and ankle, pain that increases with activity, and difficulty walking for long periods of time. You may experience difficulty standing, pain on the outside of the ankle, and bony bumps on the top of the foot and inside the foot. You may also have numbness and tingling of the feet and toes (may result from large bone spurs putting pressure on nerves), swelling, a large bump on the sole of the foot and/or an ulcer (in diabetic patients). Diabetic patients should wear a properly fitting diabetic shoe wear to prevent these complications from happening.
Diagnosis
Perform a structural assessment of the foot and ankle. Check the ankle for alignment and position. When it comes to patients with severe PTTD, the deltoid has failed, causing an instability of the ankle and possible valgus of the ankle. This is a rare and difficult problem to address. However, if one misses it, it can lead to dire consequences and potential surgical failure. Check the heel alignment and position of the heel both loaded and during varus/valgus stress. Compare range of motion of the heel to the normal contralateral limb. Check alignment of the midtarsal joint for collapse and lateral deviation. Noting the level of lateral deviation in comparison to the contralateral limb is critical for surgical planning. Check midfoot alignment of the naviculocuneiform joints and metatarsocuneiform joints both for sag and hypermobility.
Non surgical Treatment
Patients can be treated non-surgically with in-shoe devices and braces to hold their feet in the correct position. This can reduce pain and damage and assist with walking. Physical therapy is also given to improve muscle strength and help prevent injury to the foot. Surgery can be performed if the patient doesn?t find any relief. .jpg)
Surgical Treatment
Many operations are available for the treatment of dysfunction of the posterior tibial tendon after a thorough program of non-operative treatment has failed. The type of operation that is selected is determined by the age, weight, and level of activity of the patient as well as the extent of the deformity. The clinical stages outlined previously are a useful guide to operative care (Table I). In general, the clinician should perform the least invasive procedure that will decrease pain and improve function. One should consider the effects of each procedure, particularly those of arthrodesis, on the function of the rest of the foot and ankle.
Achilles Tendon Stretch Socks
 Achilles tendinitis (or Achilles tendonitis) is a strain of the Achilles tendon, which connects the calf muscles to the heel bone. Pain can be moderate or severe, but the condition is not usually serious. Of course, if you are suffering the leg and heel pain it brings, it certainly feels serious enough.
Achilles tendinitis (or Achilles tendonitis) is a strain of the Achilles tendon, which connects the calf muscles to the heel bone. Pain can be moderate or severe, but the condition is not usually serious. Of course, if you are suffering the leg and heel pain it brings, it certainly feels serious enough.
Causes
Achilles tendinitis is caused by repeated stress to the tendon, not a direct injury. Often times, this can happen from doing too much too soon and not giving your body enough time to rest or adjust to the increase in intensity or amount of exercise. Another contributing factor can be tight calf muscles. Having tight calf muscles and starting an activity can put added stress on the achilles tendon.
Symptoms
The primary symptom of Achilles tendon inflammation is pain in the back of the heel, which initially increases when exercise is begun and often lessens as exercise continues. A complete tear of the Achilles tendon typically occurs with a sudden forceful change in direction when running or playing tennis and is often accompanied by a sensation of having been struck in the back of the ankle and calf with an object such as a baseball bat.
Diagnosis
On examination, an inflamed or partially torn Achilles tendon is tender when squeezed between the fingers. Complete tears are differentiated by sudden, severe pain and inability to walk on the extremity. A palpable defect along the course of the tendon. A positive Thompson test (while the patient lies prone on the examination table, the examiner squeezes the calf muscle; this maneuver by the examiner does not cause the normally expected plantar flexion of the foot).
Nonsurgical Treatment
Ask your Pharmacist for advice. 1) Your Pharmacy stocks a range of cold packs which may be applied to the area to decrease inflammation. 2) Ask your Pharmacist about a temporary heel raise or pad which can be inserted into footwear to decrease the force absorbed by the tendon when the feet land heavily on the ground. 3) Gently massaging a heat-producing liniment into the calf can help to relieve tension in the muscle which may relieve the symptoms of Achilles Tendinitis. Ask your Pharmacist to recommend the most appropriate type. 4) Gels, sprays or creams which help to reduce inflammation are available and may be applied to the injured area. Ask your Pharmacist for advice. 5) Your Pharmacist can advise you on analgesic, anti-inflammatory medications such as Aspirin which may be of assistance. Aspirin should be avoided in children under the age of 12 and those aged 12 to 15 who have a fever. 6) Strapping the ankle can help restrict movement and minimise further injury. Your Pharmacist stocks a range of athletic strapping tape and ankle guards which may assist your injury.

Surgical Treatment
Chronic Achilles tendon tears can be more complicated to repair. A tendon that has torn and retracted (pulled back) into the leg will scar in the shortened position over time. Restoring normal tendon length is usually not an issue when surgery is performed within a few weeks of the injury. However, when there has been a delay of months or longer, the treatment can be more complicated. Several procedures can be used to add length to a chronic Achilles tear. A turndown procedure uses tissue folded down from the top of the calf to add length to the Achilles tendon. Tendon transfers from other tendons of the ankle can also be performed to help restore function of the Achilles. The results of surgery in a chronic situation are seldom as good as an acute repair. However, in some patients, these procedures can help restore function of a chronically damaged Achilles.
Prevention
By properly training the body, an athlete can build the strength of their tendons and muscles. Following a workout and dieting plan, the body will be able to build muscle and strengthen most effectively. Additionally, doing the following can prevent tendinitis. Wearing appropriate shoes will give your foot the support it needs for proper movements of the foot and ankle. Improper movements will put additional stress on your body. Stretching before an athletic activity, Stretching primes the body for a taxing activity. Additionally, this will get your blood flowing and reduce the risk of pulling a muscle. Ask your doctor about orthotics, Custom orthotics can help get your foot into proper alignment. If the foot does not execute proper mechanics, the body will adjust which will cause pain and increase the chances of injury.